Improving anti-coagulant prescribing in Warrington
Background
Direct oral anti-coagulants (DOAC) have now increased greatly as one treatment choice over the alternative warfarin. This is because they do not require the intense monitoring needed for warfarin. Patients on a DOAC will only require more routine monitoring once a year or every three months, depending on their renal function. Risks that need to be considered with taking a DOAC include under or over coagulation and continuing treatment for longer than necessary. It is important to check that those prescribed for atrial fibrillation (AF) are correctly read-coded to be on the AF register for their practice in order to ensure correct follow up.
Action
In each Warrington practice, our MMO team conducted a review of all patients taking any of the four DOAC medicines currently prescribed across the CCG. They looked specifically at the risk factors with DOACs. These included indication, dose and duration of therapy, as patients may remain on the incorrect dose for the indication or a longer treatment length than necessary. Duration of treatment, and stop dates for courses, were documented in patient notes. Patients’ renal function and weight was reviewed for dose prescribed and amended as appropriate.
The team checked any drug interactions and also for appropriateness of medication for indication/risk factors ensuring the clinical indication was clearly documented by read code in the GP system.
For this project, the team created bespoke searches and numerical filters to show all existing values relating to DOAC monitoring.
The DOAC review was started in March 2018 across 27 GP practices in Warrington. The table below shows the interventions that were made by the MMO team:
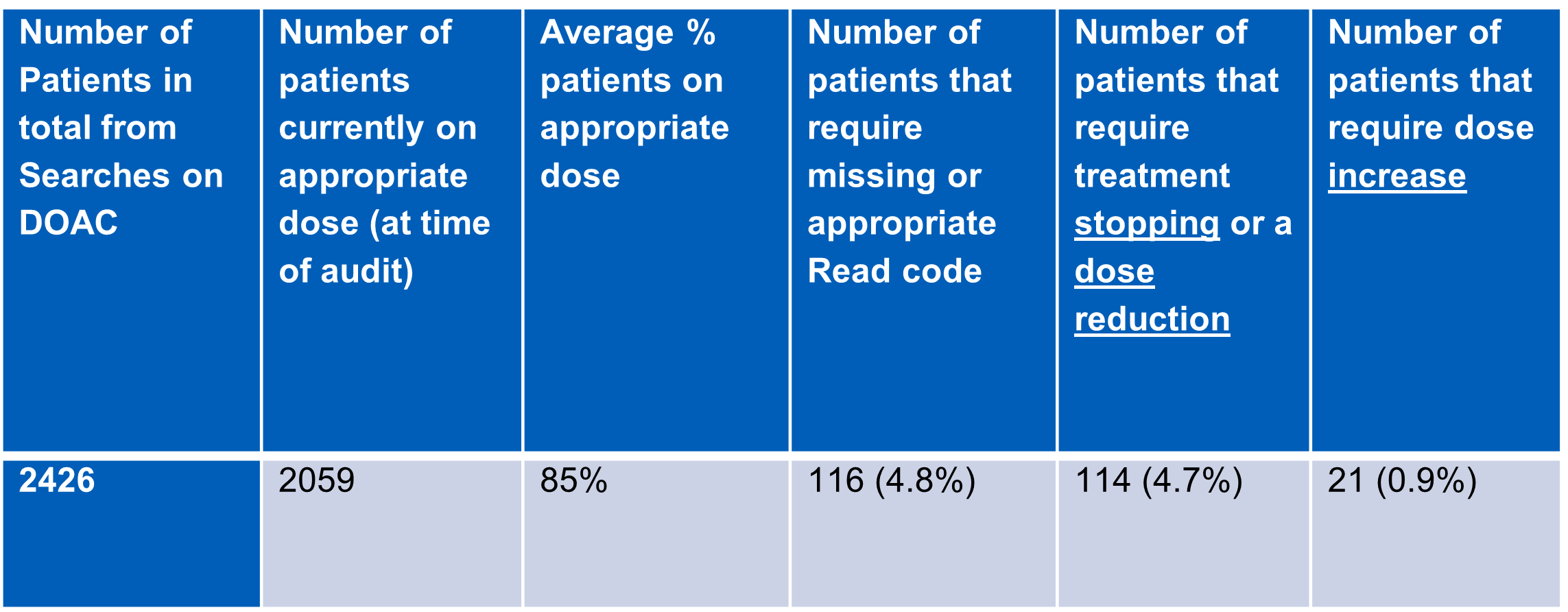
In addition to the safety aspect of this work there were £9,000 cost savings made in total.
Further information
- If there was a dose reduction required for patients on apixaban this could have a cost impact, but better patient safety.
The summary of information found during this review which if improved will improve patient care for the future includes:
1.An AF resolved read code used, if the consultation starts with a prior problem of AF [TPP looks for last read code added which is resolved] therefore the patient will NOT be on QOF AF register
2.If patients are NOT on AF register (see above) then this is not cascaded through to GRASP-AF
3.PE and DVT read codes are missing, although free text in patient notes
4.No diary (EMIS) or recall (TPP) dates used to review patients at specific times e.g. age>= 80 or weight <60Kg
5.Weight of patient missing frequently, so appropriate dose difficult to establish
6.Weight of patient in information from hospital letters but this is not added onto clinical system or there is no confirmed weight of patient on discharge letter to confirm the prescribed dose
7.Lack of clinical system protocols to guide prescribers through the add drug>indication>length of treatment?>diary/recall to review
8.Require creation of Concepts (EMIS) Alerts (TPP) to flag up patients when criteria changed e.g. age/weight/CrCl
9.Found that when patients turn 80years old, apixaban dose was routinely reduced to 2.5mg bd [without taking other criteria like weight into consideration]
10.Recording of creatinine clearance in notes but eGFR not calculated to confirm appropriate dose
11.Confusion by GP's regarding whether to use CrCl or eGFR
12.Drug monitoring requirements not up to date
13.Discharged from hospital on the lower dose of apixaban but no indication noted as reasons why they are on this lower dose e.g. no record of AKI, no recorded weight
14.Patients on DOACs that are outside the licensed indications e.g. apixaban with AF but no other indicator - Hypertensive/75+/HF etc
15.DOACs (on TPP are linked to AF as coded) but not linked to PE/DVT as frequently
16.Patient HASBLED score of 1 are put on DOACs, as age 65+ is used
Recommendations to move forward:
- MLCSU develop a DOAC protocol and template for the clinical systems that guides the prescriber through a series of yes and no questions when the drug is selected to add to the patients record
- Adding a recall/diary date to review patient if DOAC should have a specific treatment length
- Create a search to identify patients that are due the review in the coming months
- The template will require adding current values for decision making with regards to patients’ dose
- The template uses concepts to determine if the patient has the correct criteria for each DOAC e.g. hypertensive, diabetic etc to aid the prescriber
- MLCSU to develop a clinical system alert to any changes noted in the patients’ records such as
- Age, in particular, those reaching 80years old, any change in weight or eGFR (CrCl)

